COPD - Chronic Obstructive Pulmonary Disease
COPD is the name for a group of lung diseases that make it hard for you to breathe.
What is COPD?
What are the causes of COPD?
What are the signs and symptoms of COPD?
What are the possible tests to detect COPD?
What are the possible procedures and treatments for COPD?
What is the future plan if you have COPD?
What is COPD?
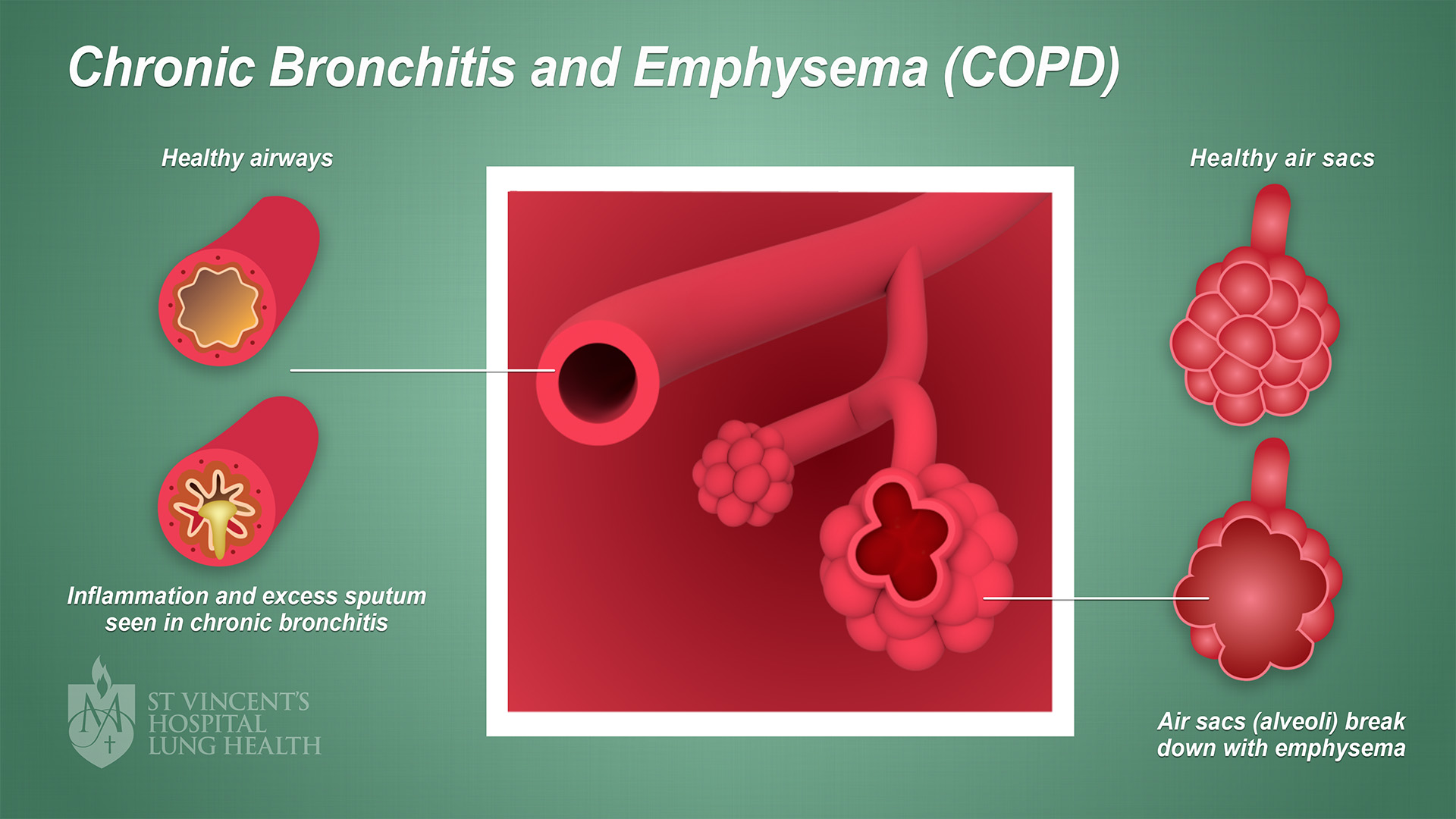
COPD stands for Chronic Obstructive Pulmonary Disease. COPD refers to two types of lung disease:
- Chronic bronchitis – when the airways (the tubes that carry air into and out of your lungs) become partly blocked from swelling or mucus and you cough up phlegm
- Emphysema – when the air sacs which exchange gases at the end of your airways become damaged and enlarged, making it difficult to breathe.
When you have COPD, your airways become swollen and sometimes they get clogged with mucus. You can't get enough fresh oxygen with each breath. You also find it difficult to push out the air.
The image below illustrates COPD. (Click image to enlarge)
What are the causes of COPD?
Smoking is the most common cause of COPD. But, non-smokers can also get COPD. People who have been exposed to dusts can get COPD from dust inhalation. Second-hand smoke, also called passive smoking, is also a risk factor for COPD.
Other causes of COPD are:
- Asthma – asthma that is not well controlled over a long period of time can lead to COPD
- Infections – a disease called tuberculosis can lead to COPD
- Pollution and fumes – including air pollution or breathing in chemical fumes, dusts or toxic substances.
In rare cases, people with COPD can have faults in their genes (the instruction manuals for how your body develops and works). These faults include a disease called “alpha-1 antitrypsin deficiency” or AAT deficiency. People with AAT deficiency don't have enough of a protein needed to protect their lungs from damage.
What are the signs and symptoms of COPD?
Often, COPD develops slowly. Symptoms can come on over time, and it can be years before you notice symptoms. The most common sign of COPD is a cough that produces regular clear phlegm. It is not normal to cough up phlegm regularly.
Another common symptom is breathlessness. You may start to feel out of breath during exercise or when you’re carrying something, and this feeling may slowly get worse.
Shortness of breath is never normal, so see your doctor if you notice this symptom.
Other signs of COPD include:
- A cough that doesn't go away
- Blue lips or fingernails
- Coughing up lots of mucus (sputum or phlegm)
- Extreme tiredness most or all of the time
- Repeated chest infections
- Shortness of breath when you’re physically active
- Tightness in the chest
- Wheezing.
What are the possible tests to detect COPD?
If your doctor thinks you may have COPD, you will be asked about:
- How long you have had your symptoms
- Your exposure to dusts, fumes or vapours.
- Your family history of COPD
- Your medical history
- Your symptoms.
Your doctor will then recommend several tests in order to get the right diagnosis. COPD has similar symptoms to several other lung diseases, including:
Your doctor will listen to your chest using a stethoscope. A stethoscope is the instrument your doctor often wears around her/his neck.
Your doctor will place the stethoscope on your chest to listen for any unusual sounds, such as wheezing. Based on what your doctor hears, you may need one or more lung function tests.
The most common lung function test is called spirometry. This test measures the amount of air you can breathe out.
In a spirometry test:
- You will be asked to take a deep breath
- You’ll blow hard into a mouthpiece connected to a small machine called a spirometer
- The spirometer will measure how fast you blow air out of your lungs
- You will inhale a treatment called salbutamol through a special plastic bubble, and your doctor will see if much your lungs improve.
A spirometry test will tell you:
- How much air you breathe out in six seconds, called the forced vital capacity (FVC)
- How much of air came out in the first second, called the forced expiratory volume (FEV1).
Other tests to diagnose COPD include:
- Alpha-1 Antitrypsin Deficiency Testing – another type of blood test which checks for a protein called AAT (people who lack AAT are more likely to get lung diseases earlier than usual, at around 30 to 40 years old)
- Arterial blood gas test – a simple blood test measuring amount of oxygen and carbon dioxide in your blood (a lack of oxygen in your bloodstream can be a sign of COPD)
- Chest CT scan – you will lie underneath a CT scanner, a machine shaped like a tunnel, which will take more detailed images of your heart, lungs and blood vessels
- Chest X-ray – an X-ray machine will take images of your chest to look for the presence of lung disease
- Complex lung function tests – you will sit in a transparent box and breathe in and out to measure how much air is in your lungs.
What are the possible procedures and treatments for COPD?
While there is no cure for COPD, there are treatments to help manage symptoms. It’s important that you treat your symptoms so the disease doesn’t get worse.
Quitting smoking is the most important step for treating COPD. No one with COPD should smoke, and even smoking a few cigarettes a day is harmful. Quitting smoking will support your lungs and improve your long-term health. Talk to your doctor about support to help you quit.
Your doctor will also want to prevent or treat any complications related to COPD.
Doctors use stages (or grades) to describe how severe your COPD is. Your grade will determine your treatment plan.
Your treatment plan may include any of the following:
- Antibiotics – medicines that fight bacterial infections
- Bronchodilators – inhaled medicines that help to open your airways
- Corticosteroids – medicines that reduce inflammation and swelling in your airways
- Flu or pneumonia vaccines – vaccines that lower your risk for getting the flu or pneumonia
- Oxygen therapy – oxygen can help to reduce shortness of breath, protect your organs and enhance your quality of life (however, oxygen is not needed for everyone with COPD)
- Pulmonary rehabilitation – a graded exercise course run by special lung physiotherapists
- Surgery – in severe cases, your doctor may suggest surgery to remove diseased lung tissue or replace a diseased lung with a healthy one.
If you are prescribed an inhaler (or puffer), it's important to use it correctly so that your lungs can benefit from the medication. Read through the National Asthma Council of Australia's Inhaler Checklist to see if you are using your puffer correctly.
There are many steps you can take to help improve your quality of life, including:
- Avoid smoke – as well as fumes, dust and air pollution
- Avoid spicy foods – or any foods that give you indigestion
- Eat a healthy diet – speak to your doctor or a dietitian about a healthy eating plan
- Get regular check-ups – don’t miss any appointments
- Get vaccinated every year – flu and the common cold can make your lungs much worse
- Learn breathing exercises – this will help you to manage your symptom
- Quit smoking – if you smoke, one of the most important things for all your health is to stop so chat with your medical team about getting started
- Take your medications as directed – speak with your doctor if you have any questions and ensure you know how to use your inhalers
- Walk or do other light exercises – aim to exercise several times a week.
Below, you can watch a video about good nutrition for people with chronic lung conditions.
What is the future plan if you have COPD?
Your doctor will give you guidance and instructions on how to manage your condition. The future plan will include the following steps:
- Join a pulmonary rehabilitation service – in a rehabilitation service, a team of health professionals can teach you about how to manage your COPD and monitor your condition, covering exercise, disease management, and counselling to help you stay as healthy and active as possible
- Follow your dedicated treatment plan – always take your medicines, continue to make healthy lifestyle changes, stay active and go to your regular medical appointments
- See a dedicated lung nurse – your medical team can help and arrange extra nursing support or care at home, so ask your doctor about this.
Know when to seek help
Phone triple zero (000) or seek urgent medical help if:
- You breathe too fast and hard, even when taking medicines
- You can't walk or talk because you are so breathless
- You have severe shortness of breath
- Your heart beats very fast or it has an irregular beat
- Your lips or fingernails turn blue.