LAM (Lymphangioleiomyomatosis)
Lymphangioleiomyomatosis (pronounced lim-FAN-je-o-LI-o-MI-o-ma-TO-sis), or LAM for short, is a rare lung disease.
What is LAM?
What are the causes of LAM?
What are the signs and symptoms of LAM?
What are the possible tests to diagnose LAM?
What are the possible procedures and treatments for LAM?
What is the future plan if you have LAM?
What is LAM?
LAM is a rare lung disease characterised by abnormal cell growth in the smooth muscle tissue of the lungs and the abdomen. LAM affects almost only women. The average age people develop LAM is 35.
What are the causes of LAM?
LAM is a rare form of low-grade cancer. Low-grade cancer cells look more like normal cells under a microscope, and they often grow and spread slowly. In LAM, myofibroblasts (muscle and fibrous tissue cells) move from the uterus through the lymph channels to other organs such as the lung and abdominal lymph nodes. LAM occurs in people who have a gene mutation of the TSC2 gene. The hormone oestrogen promotes the growth of LAM cells.
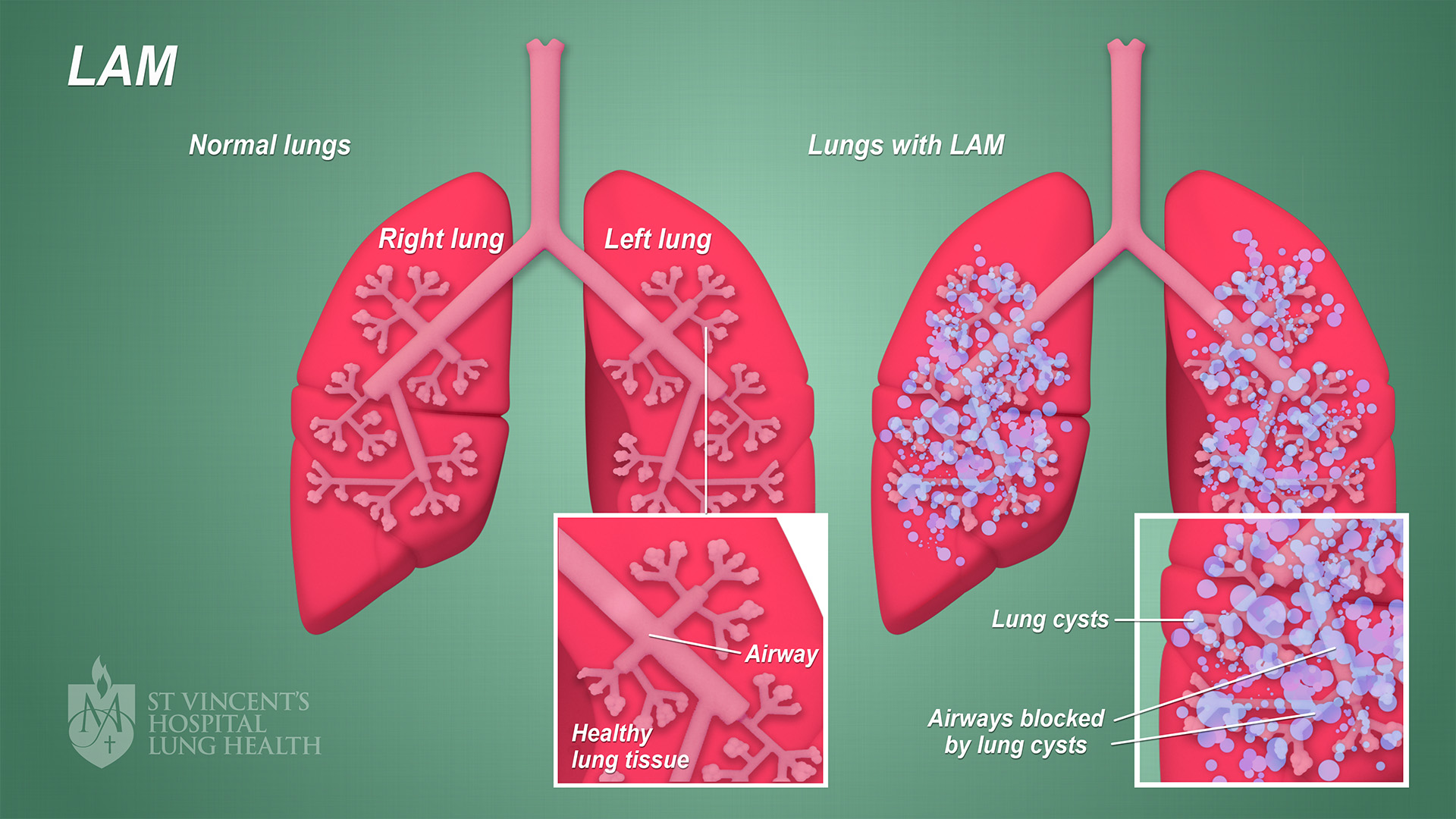
LAM results in abnormal growth of smooth muscle cells which damage and block the small airways of the lungs. As a result:
- Airflow is reduced
- Blood vessels are blocked, especially veins
- Cysts form
- Transport of oxygen is reduced.
The image below illustrates LAM. (Click on the image to enlarge)
There are two types of LAM:
- Sporadic LAM (S-LAM)
- Tuberous Sclerosis LAM (TSC-LAM) – which occurs in women who have a rare disease called Tuberous Sclerosis Complex (TSC).
What are the signs and symptoms of LAM?
LAM almost always affects women and starts around age 35. Women with LAM may have symptoms for a few years before they are diagnosed.
Signs and symptoms of LAM include:
- Chest ache or pain that can worsen with inhalation (breathing in)
- Chronic cough with bloody mucus
- Fatigue
- Shortness of breath which gets worse over time.
Cysts in the lungs are an important sign of LAM. Cysts can rupture and cause a pneumothorax (when air leaks from the lung into the pleural space). This rupture also causes shortness of breath as well as pain in the chest, back and shoulder.
What are the possible tests to diagnose LAM?
LAM is difficult to diagnose. Symptoms of LAM are similar to those of other lung disorders such as asthma, bronchitis and emphysema.
Tests to diagnose LAM include:
- Arterial Blood Gas (ABG) test – a sample of blood is taken from an artery to measure the amount of gases (oxygen and carbon dioxide) in your blood
- Biopsy of the lung – a small sample of lung tissue is tested and may provide a more accurate diagnosis of LAM
- Chest Computed tomography (CT) – an X-ray is taken to detect changes and cyst-like structures in the chest, pelvis, kidney and lymph structures
- Pulse Oximetry (SaO2) – a small clip with a sensor is placed on the tip of your finger to measure the amount of oxygen in your blood
- Six Minute Walk Test – oxygen levels and heart rate are measured while you walk for a period of 6 minutes
- Thoracentesis – a needle is inserted into the space between your lung and chest wall in order to take a sample of fluid for testing.
What are the possible procedures and treatments for LAM?
There is no cure for LAM. However, there are a number of treatments to help manage symptoms. Current treatment options include:
- Medication – certain drugs can help improve lung function and may assist in managing symptoms; your LAM specialist will talk to you about the drugs that may be right for you
- Oxygen therapy – supplying the tissue and organs with oxygen can help to ease symptoms in people with more advanced cases of LAM
- Pleurodesis – a procedure which sticks the lung to the chest cavity to try and prevent the lung from collapsing and to prevent fluid build-up in the cavity; pleurodesis is recommended for women who have already had one lung collapse (pneumothorax)
- Thoracotomy – a surgical procedure where an incision is made in the chest to access the lungs
- Thoracoscopy or VATS (Video-assisted Thorascopic Surgery) – a procedure that uses a small fibre-optic camera, inserted via a small incision in the side, to gain access to your chest; it is a less invasive procedure than a thoracotomy
- Lung transplant – an option for advanced LAM cases.
What is the future plan if you have LAM?
As more people are being diagnosed earlier, and technology is advancing, people with LAM are living longer. If you or someone you know has LAM, the following steps can help:
- Emotional support – having a support group or a strong network of friends and family are essential in managing your condition; support can also help reduce any feelings of fear, anxiety, depression and stress
- Lifestyle changes – living a healthy lifestyle which includes not smoking, exercising regularly and eating a healthy, balanced diet is important, so speak to your doctor to discuss lifestyle changes that are right for you
- Pregnancy and birth control planning – pregnancy and birth control pills containing oestrogen can make symptoms of LAM worse due to changes in hormones (talk to your doctor about your options)
- Pulmonary rehabilitation – regular exercise is recommended to people who have LAM, and a pulmonary rehabilitation program, supervised by trained professionals who monitor oxygen and heart rate levels while you exercise, is a good way to safely exercise
- Specialist care – a healthcare professional who specialises in respiratory care or lung diseases can help to monitor your health and treatment plan; specialists also have access to new drugs and therapies that can help stabilise LAM
- Vaccines – talk to your doctor about your vaccine status and ensure you are up to date with vaccinations for both the flu (influenza) and pneumonia (pneumococcal).