PE (Pulmonary Embolism)
A pulmonary embolism is a type of blood clot that is found in your lungs.
What is a PE?
What causes a PE?
What are the signs and symptoms of a PE?
What are the possible tests to diagnose a PE?
What are the possible procedures and treatments for PE?
What is the future plan if you have a PE?
What is a PE?
A pulmonary embolism is a type of blood clot that is found in your lungs.
What causes a PE?
A pulmonary embolism is often caused by one or more blood clots (called deep vein thrombosis (DVT). The clot travels from your leg or arm to a main artery (known as the pulmonary artery) in your lungs.
The ability for your blood to clot is a normal function, typically as a response to an injury (to prevent excessive blood loss). However, in some cases blood clots can cause complications.
When a blood clot travels to your lungs it can result in serious damage. A blood clot can reduce the amount of oxygen in your body and can damage your lungs and other organs. A pulmonary embolism is a medical emergency, and it can be fatal (cause death).
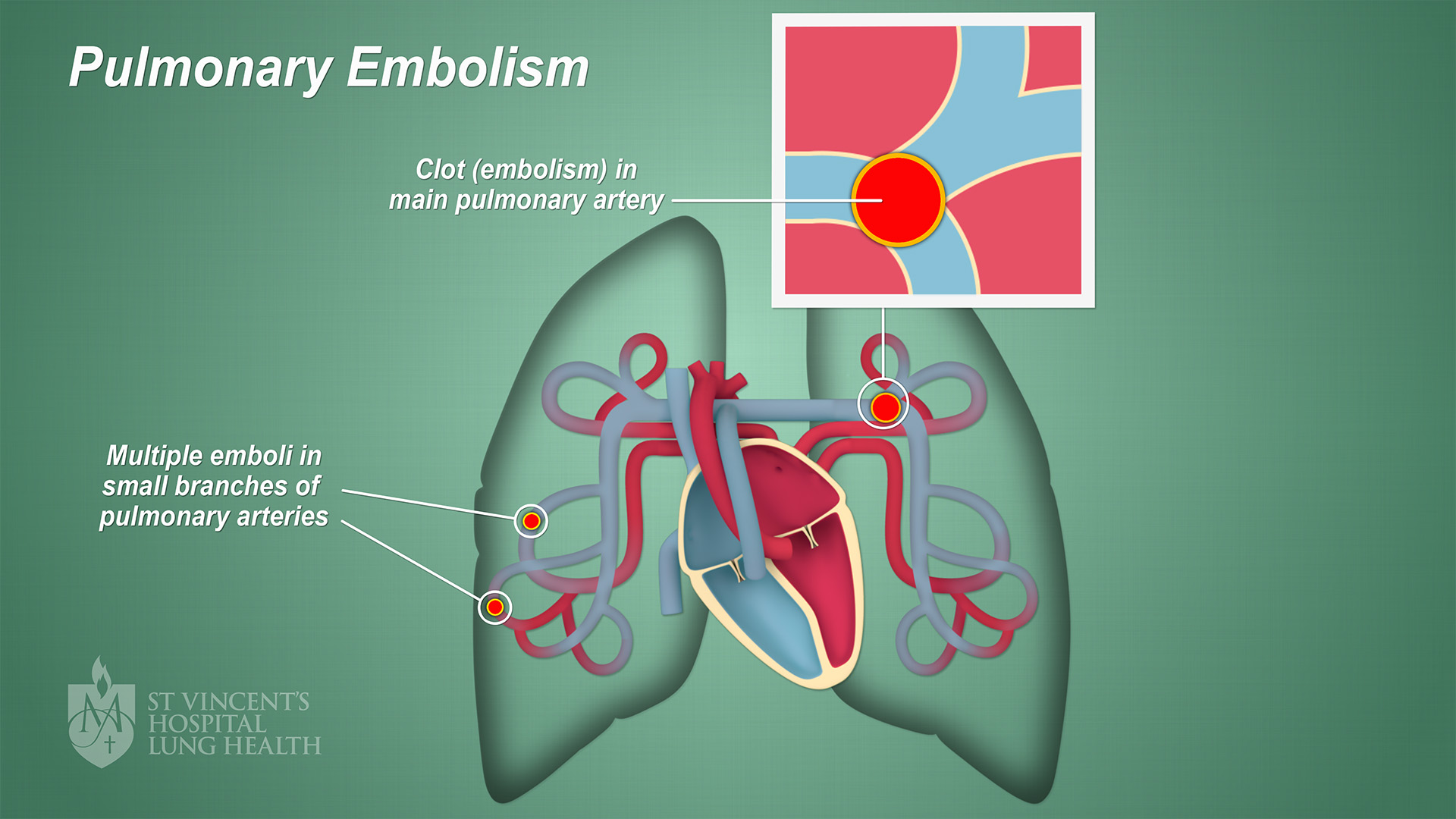
The image below illustrates pulmonary embolism. (Click on image to enlarge)
The risk factors for a pulmonary embolism include:
- Damaged blood vessels – blood vessels that have been damaged or injured due to trauma can increase your risk for clots
- Hypercoagulability – is a term to describe the increased ability of your blood to form clots, which can happen as a result of some medications (such as birth control pills), smoking, cancer, pregnancy and recent surgery
- Immobility – blood clots can result from long periods of rest or lack of movement, such as on long flights or if you have had long periods of bed rest due to illness or surgery.
In rare cases, a blockage in the pulmonary artery can be a result of something other than a blood clot, like an air bubble or tumour.
What are the signs and symptoms of a PE?
Symptoms of a pulmonary embolism typically come on suddenly, and you should seek urgent medical attention if you experience the following:
- A cough, which may contain blood
- A heavy feeling in your chest, or chest pain
- Dizziness or a feeling of being ‘light-headed’
- Pain in your back
- Rapid heart rate
- Shortness of breath
- Sweating that is more than usual.
Symptoms of a DVT include the following:
- An area on either an arm or leg that feels warm or hot to touch
- Leg pain or tenderness, particularly in the calf
- Redness of the skin in the affected arm or leg
- Swelling in either an arm or leg
- Veins in your arm or leg that are larger than normal.
If a DVT is found earlier enough, doctors can reduce the risk of a pulmonary embolism. It is important that you seek urgent medical attention if you experience any of the above DVT symptoms as well.
What are the possible tests to diagnose a PE?
Typically your doctor will talk through your symptoms as well as examine you. You will most likely require a number of tests, which could include:
What are the possible procedures and treatments for PE?
- Anticoagulants – also called blood thinners, they are the most common treatment for PE, helping to dissolve the blood clot and prevent future blood clots forming (common blood thinners prescribed include warfarin and heparin; these medications used to require regular blood tests to make sure that the blood is thin enough, but there are now new anticoagulants that do not need regular blood test monitoring)
- Inferior vena cava filter (IVC) – a filter that catches the blood clot before it reaches the heart and lungs; the filter is inserted in the inferior vena cava, which is a large vein that carries blood to the heart
- Surgery – to remove the blood clot in very serious cases, called a pulmonary thromboendarterectomy
- Thrombolytics – these medicines break down and dissolve the blood clot.
What is the future plan if you have a PE?
If you have had a pulmonary embolism, the following options may help reduce your risk of a blood clot forming in the future:
- Compression stockings – knee-high socks that apply a firm pressure about your legs when worn and help your blood circulate (move) in your legs
- Exercise – regular movement or your arms and legs help keep your blood flowing and prevent it ‘pooling’ in your lower legs
- Hydration – drinking plenty of fluids prevents you becoming dehydrated (which can thicken your blood and increase the risk for blood clots)
- Maintain a healthy weight – if you are overweight or obese, talk to your doctor about a referral to a registered nutritionist or dietitian
- Medication – such as blood thinners (known as anticoagulants) will help prevent your blood from forming clots
- Smoking – if you smoke, talk with your doctor about quitting
- Stretches – regular stretches and leg movement when on long trips (such as flights) can help keep your blood circulating.