PE (Pleural Effusion)
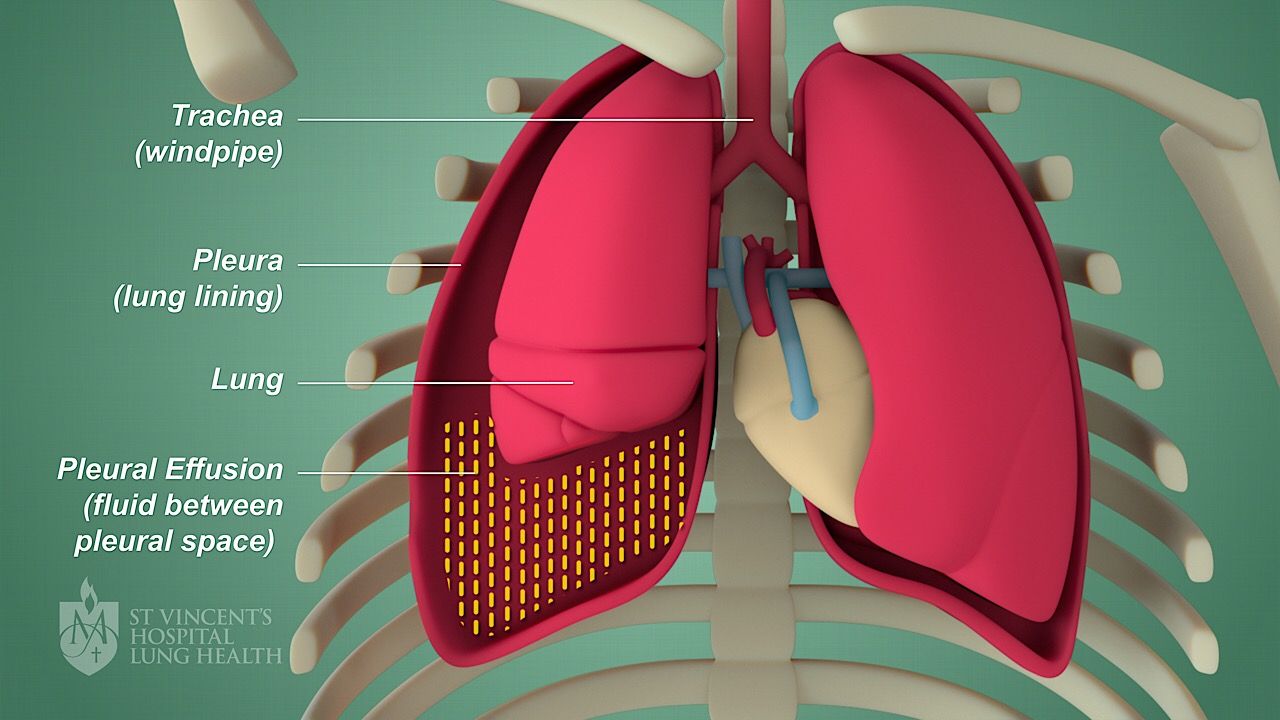
A pleural effusion is an excess amount of fluid around the lungs.
What is a pleural effusion?
What are the causes of a pleural effusion?
What are the signs and symptoms of a pleural effusion?
What are the possible tests to detect a pleural effusion?
What are the possible procedures and treatments for a pleural effusion?
What is the future plan if you have a pleural effusion?
What is a pleural effusion?
Everyone has a small amount of fluid between the lung and the chest wall (the pleural space).
Sometimes, the healthy balance of this fluid can be disturbed. A pleural effusion is when your lungs are releasing (secreting) too much fluid and not reabsorbing enough.
Excess fluid can compress the lungs, causing shortness of breath.
The image below shows a pleural effusion. (Click image to enlarge)
There are two types of pleural effusions: transudative and exudative.
- Exudative pleural effusion – caused by inflammatory conditions such as lung infections or tumours; this type of pleural effusion tends to be more challenging to treat as it is more serious than a transudative pleural effusion
- Transudative pleural effusion – fluid leaks into the pleural space; this type of pleural effusion is usually a result of conditions such heart failure or cirrhosis of the liver.
What are the causes of a pleural effusion?
There are many causes of a pleural effusion. Depending on the cause, your doctor will determine the treatment option. Common causes include:
- Autoimmune disorders – rheumatoid arthritis or lupus can cause pleural effusions
- Cancer – lung cancer as well as other cancers that have spread to the lung can also result in a pleural effusion
- Cirrhosis of the liver – when severe scarring has occurs in the liver due to long term exposure to certain substances such as alcohol, the liver's function is severely impaired, resulting in a build-up of fluid in the pleural space
- Congestive heart failure (CHF) – the most common cause of a pleural effusion, CHF occurs as a result of poor heart function and a decreased ability for the heart to pump blood effectively
- Infections – some diseases caused by viruses or bacteria such as pneumonia or tuberculosis can also lead to a pleural effusion
- Previous surgery – a pleural effusion is reasonably common after either heart surgery (often Coronary Artery Bypass Grafting or LVAD implantation) or any lung surgery in that side of the chest
- Pulmonary embolism – a blood clot causes a blockage in one of the lungs, which can result in a pleural effusion as a result of poor lung function.
What are the signs and symptoms of a pleural effusion?
Symptoms of a pleural effusion can be different for everyone. Larger-sized pleural effusions are more likely to show symptoms, which can include:
- A cough
- Chest pain, particularly when taking a deep breath (also known as pleuritic pain or pleurisy)
- Difficulty catching your breath
- High temperature
- Trouble breathing when lying down.
What are the possible tests to detect a pleural effusion?
To confirm a pleural effusion, your doctor will do a physical examination, as well as ask about your symptoms and order tests, such as:
- Chest X-ray – pleural effusions will show up as a white mass on X-rays, while air space looks black; if your doctor suspects a pleural effusion is likely, he may request further X-rays to determine if the fluid in the pleural space moves freely
- Chest ultrasound – a probe is used to generate images of the chest; an ultrasound can also provide a detailed location of where the fluid is in the pleural space to obtain a sample for testing
- Computed tomography (CT scan) – a CT scan provides a more detailed picture of the chest compared with a chest X-ray, as it builds images of both the inside and outside of the chest
- Thoracentesis – your doctor inserts a needle into the pleural space to test a sample of the fluid.
What are the possible procedures and treatments for a pleural effusion?
The cause of the pleural effusion will determine the treatment option.
For example, if pneumonia is the cause, then a course of antibiotics will be required. If congestive heart failure is the cause, diuretics (which increase your production of urine) may be prescribed.
Other procedures and treatments include:
- Chest drainage – where a small cut to be made in the chest and a small plastic tube is inserted into the pleural space to help drain fluid. This treatment is beneficial for large, inflamed or infected pleural effusions
- Non-steroidal anti-inflammatory drugs (NSAIDs) – medications that help reduce swelling, fever and pain
- Pleurodesis – keyhole surgery, performed through a 1.5cm incision. The fluid is suctioned out of the chest, and talc powder is sprayed into the chest space to get the lung to stick to the chest wall so that the fluid can’t re-accumulate.
What is the future plan if you have a pleural effusion?
The type, cause and size of your pleural effusion will determine the length of your hospital stay and recovery time.
It is common to feel tired and weak in the first week after leaving hospital. You may require ongoing care and medical check-ups once you are home.
Here are some extra tips to help your body recover after a pleural effusion:
- Continue to take your medications as prescribed – talk with your doctor about pain medications that contain acetaminophen, as this can cause liver damage
- Don’t smoke or breathe in second-hand smoke – this increases your risk for lung infections and can make it difficult for you to breathe
- Practice breathing exercises – deep breathing and coughing help decrease the risk for lung infections and open your airways. Breathe deeply in, holding it for as long as possible, then let the air out, coughing at the end.
Contact your medical team, at any time, if you are concerned or notice the following symptoms:
- A bluish tinge to your lips or fingernails
- Cough up bloody mucus, or mucus that is yellow, green or grey
- Constant pain, or pain that gets worse
- Difficulty breathing
- Feeling faint or dizzy, and cannot concentrate
- High temperature.